Vitamin D levels in cells, not blood, is important (IVF follicular fluid in this case)
Low vitamin D levels in follicular fluid, but not in serum, are associated with adverse outcomes in assisted reproduction
Arch Gynecol Obstet. 2021 Aug 8. doi: 10.1007/s00404-021-06174-9
Kahindo P Muyayalo # 1 2, Su Song # 3, Hui Zhai # 4, Hong Liu 1, Dong-Hui Huang 1, Hui Zhou 1, Yang-Jiao Chen 3, Ai-Hua Liao 5
Purpose: To assess the relationship between serum/follicular fluid (FF) vitamin D (VD) status and assisted reproductive technology (ART) treatment outcomes among infertile patients.
Methods: A prospective cohort study, including 132 infertile patients scheduled for their first ART treatment cycle, was carried out in a Reproductive Medical Center. Serum and FF samples were collected to assess 25-hydroxy VD [25(OH)D] levels. Low VD level was defined as 25(OH)D concentration of less than 30 ng/mL.
Results: Most infertile patients had low VD levels in serum (88%) and FF (90%). We observed a moderately positive correlation between VD levels in serum and FF (r = 0.34, p < 0.0001). Compared to the group of patients with low VD levels in the FF, those with sufficient VD levels had a significantly higher number of retrieved oocytes (p = 0.03), normal fertilization (p = 0.01), and high-quality embryos (p = 0.001). Moreover, patients with sufficient VD levels in the FF also had significantly higher implantation rates than those with low VD levels (76.92% vs. 46.58%, respectively, p = 0.01) and clinical pregnancy rates (92.31% vs. 61.54%, respectively, p = 0.04).
Conclusion: These data collectively revealed that low VD levels in serum and FF were common among infertile patients.
VD levels in FF, but not in serum, were associated with:
embryo quality,
normal fertilization,
implantation rates, and
clinical pregnancy rates.
Further studies are mandatory to determine the molecular mechanism and VD's potential therapeutic benefits in infertile patients.
References
Christakos S, Dhawan P, Verstuyf A, Verlinden L, Carmeliet G (2016) Vitamin D: metabolism, molecular mechanism of action, and pleiotropic effects. Physiol Rev 96(1):365–408. https://doi.org/10.1152/physrev.00014.2015 - DOI - PubMed
Di Rosa M, Malaguarnera G, De Gregorio C, Palumbo M, Nunnari G, Malaguarnera L (2012) Immuno-modulatory effects of vitamin D3 in human monocyte and macrophages. Cell Immunol 280(1):36–43. https://doi.org/10.1016/j.cellimm.2012.10.009 - DOI - PubMed
Van Etten E, Decallonne B, Verlinden L, Verstuyf A, Bouillon R, Mathieu C (2003) Analogs of 1alpha,25-dihydroxyvitamin D3 as pluripotent immunomodulators. J Cell Biochem 88(2):223–226. https://doi.org/10.1002/jcb.10329 - DOI - PubMed
Irani M, Merhi Z (2014) Role of vitamin D in ovarian physiology and its implication in reproduction: a systematic review. Fertil Steril 102(2):460–8 e3. https://doi.org/10.1016/j.fertnstert.2014.04.046 - DOI - PubMed
Du H, Daftary GS, Lalwani SI, Taylor HS (2005) Direct regulation of HOXA10 by 1,25-(OH)2D3 in human myelomonocytic cells and human endometrial stromal cells. Mol Endocrinol 19(9):2222–2233. https://doi.org/10.1210/me.2004-0336 - DOI - PubMed
Wehr E, Pieber TR, Obermayer-Pietsch B (2011) Effect of vitamin D3 treatment on glucose metabolism and menstrual frequency in polycystic ovary syndrome women: a pilot study. J Endocrinol Invest 34(10):757–763. https://doi.org/10.3275/7748 - DOI - PubMed
Asadi M, Matin N, Frootan M, Mohamadpour J, Qorbani M, Tanha FD (2014) Vitamin D improves endometrial thickness in PCOS women who need intrauterine insemination: a randomized double-blind placebo-controlled trial. Arch Gynecol Obstet 289(4):865–870. https://doi.org/10.1007/s00404-013-3055-x - DOI - PubMed
Lasco A, Catalano A, Benvenga S (2012) Improvement of primary dysmenorrhea caused by a single oral dose of vitamin D: results of a randomized, double-blind, placebo-controlled study. Arch Intern Med 172(4):366–367. https://doi.org/10.1001/archinternmed.2011.715 - DOI - PubMed
Wise LA, Ruiz-Narvaez EA, Haddad SA, Rosenberg L, Palmer JR (2014) Polymorphisms in vitamin D-related genes and risk of uterine leiomyomata. Fertil Steril 102(2):503–10 e1. https://doi.org/10.1016/j.fertnstert.2014.04.037 - DOI - PubMed - PMC
Nair R, Maseeh A (2012) Vitamin D: the “sunshine” vitamin. J Pharmacol Pharmacother 3(2):118–126. https://doi.org/10.4103/0976-500X.95506 - DOI - PubMed - PMC
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357(3):266–281. https://doi.org/10.1056/NEJMra070553 - DOI - PubMed
Burgaz A, Orsini N, Larsson SC, Wolk A (2011) Blood 25-hydroxyvitamin D concentration and hypertension: a meta-analysis. J Hypertens 29(4):636–645. https://doi.org/10.1097/HJH.0b013e32834320f9 - DOI - PubMed
Satirapoj B, Limwannata P, Chaiprasert A, Supasyndh O, Choovichian P (2013) Vitamin D insufficiency and deficiency with stages of chronic kidney disease in an Asian population. BMC Nephrol 14:206. https://doi.org/10.1186/1471-2369-14-206 - DOI - PubMed - PMC
Ota K, Dambaeva S, Han AR, Beaman K, Gilman-Sachs A, Kwak-Kim J (2014) Vitamin D deficiency may be a risk factor for recurrent pregnancy losses by increasing cellular immunity and autoimmunity. Hum Reprod 29(2):208–219. https://doi.org/10.1093/humrep/det424 - DOI - PubMed
Rosen CJ, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA et al (2012) IOM committee members respond to Endocrine Society vitamin D guideline. J Clin Endocrinol Metab 97(4):1146–1152. https://doi.org/10.1210/jc.2011-2218 - DOI - PubMed - PMC
Kebapcilar AG, Kulaksizoglu M, Kebapcilar L, Gonen MS, Unlu A, Topcu A et al (2013) Is there a link between premature ovarian failure and serum concentrations of vitamin D, zinc, and copper? Menopause 20(1):94–99. https://doi.org/10.1097/gme.0b013e31826015ca - DOI - PubMed
Grundmann M, von Versen-Hoynck F (2011) Vitamin D—roles in women’s reproductive health? Reprod Biol Endocrinol 9:146. https://doi.org/10.1186/1477-7827-9-146 - DOI - PubMed - PMC
Ranjana H (2017) Role of vitamin D in infertility. J Public Health Policy Plann. 1:8–10
Human Fertilisation and Embryology Authority (HFEA). Fertility treatment in 2013: trends and figures. 2016. https://www.hfea.gov.uk/media/2081/hfea-fertility-trends-2013.pdf . Accessed 5 Jan 2020
Centers for Disease Control and Prevention, American Society for Reproductive Medicine, Society for Assisted Reproductive Technology. 2015 Assisted Reproductive Technology National Summary Report. Atlanta (GA): US Dept of Health and Human Services; 2017. https://www.cdc.gov/art/pdf/2015-report/art-2015-national-summary-report... . Accessed 28 Mar 2020
Chu J, Gallos I, Tobias A, Tan B, Eapen A, Coomarasamy A (2018) Vitamin D and assisted reproductive treatment outcome: a systematic review and meta-analysis. Hum Reprod 33(1):65–80. https://doi.org/10.1093/humrep/dex326 - DOI - PubMed
Ciepiela P, Duleba AJ, Kowaleczko E, Chelstowski K, Kurzawa R (2018) Vitamin D as a follicular marker of human oocyte quality and a serum marker of in vitro fertilization outcome. J Assist Reprod Genet 35(7):1265–1276. https://doi.org/10.1007/s10815-018-1179-4 - DOI - PubMed - PMC
Hornstein MD (2019) Vitamin D and infertility: the evidence. Fertility Reprod 1(1):31–33 - DOI
Lv SS, Wang JY, Wang XQ, Wang Y, Xu Y (2016) Serum vitamin D status and in vitro fertilization outcomes: a systematic review and meta-analysis. Arch Gynecol Obstet 293(6):1339–1345. https://doi.org/10.1007/s00404-016-4058-1 - DOI - PubMed
Albuquerque LE, Saconato H, Maciel MC (2005) Depot versus daily administration of gonadotrophin releasing hormone agonist protocols for pituitary desensitization in assisted reproduction cycles. Cochrane Database Syst Rev 1:CD002808. https://doi.org/10.1002/14651858.CD002808.pub2 - DOI
Xiao Y, Wang Y, Wang M, Liu K (2018) Follicular flushing increases the number of oocytes retrieved in poor ovarian responders undergoing in vitro fertilization: a retrospective cohort study. BMC Womens Health 18(1):186. https://doi.org/10.1186/s12905-018-0681-2 - DOI - PubMed - PMC
Brinsden PR (1999) A textbook of in vitro fertilization and assisted reproduction: the bourn hall guide to clinical and laboratory practice, 2nd edn. CRC Press, London
Liu X, Zhang W, Xu Y, Chu Y, Wang X, Li Q et al (2019) Effect of vitamin D status on normal fertilization rate following in vitro fertilization. Reprod Biol Endocrinol 17(1):59. https://doi.org/10.1186/s12958-019-0500-0 - DOI - PubMed - PMC
Abuzeid MI, Bolonduro O, La Chance J, Abozaid T, Urich M, Ullah K et al (2014) Cumulative live birth rate and assisted reproduction: impact of female age and transfer day. Facts Views Vis Obgyn 6(3):145–149 - PubMed - PMC
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP et al (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96(7):1911–1930. https://doi.org/10.1210/jc.2011-0385 - DOI - PubMed
Muyayalo KP, Huang XB, Qian Z, Li ZH, Mor G, Liao AH (2019) Low circulating levels of vitamin D may contribute to the occurrence of preeclampsia through deregulation of Treg /Th17 cell ratio. Am J Reprod Immunol 82(4):e13168. https://doi.org/10.1111/aji.13168 - DOI - PubMed
Chu J, Gallos I, Tobias A, Robinson L, Kirkman-Brown J, Dhillon-Smith R et al (2019) Vitamin D and assisted reproductive treatment outcome: a prospective cohort study. Reprod Health 16(1):106. https://doi.org/10.1186/s12978-019-0769-7 - DOI - PubMed - PMC
Firouzabadi RD, Rahmani E, Rahsepar M, Firouzabadi MM (2014) Value of follicular fluid vitamin D in predicting the pregnancy rate in an IVF program. Arch Gynecol Obstet 289(1):201–206. https://doi.org/10.1007/s00404-013-2959-9 - DOI - PubMed
Boz I, Teskereci G, Ozekinci M (2020) High prevalence of vitamin D deficiency in Turkish women undergoing in vitro fertilization: a descriptive study. Health Care Women Int 41(2):147–158. https://doi.org/10.1080/07399332.2019.1569015 - DOI - PubMed
Xie Q-W, Zhang M (2013) White or tan? A cross-cultural analysis of skin beauty advertisements between China and the United States. Asian J Commun 23(5):538–554. https://doi.org/10.1080/01292986.2012.756046 - DOI
Zhang W, Stoecklin E, Eggersdorfer M (2013) A glimpse of vitamin D status in Mainland China. Nutrition 29(7–8):953–957. https://doi.org/10.1016/j.nut.2013.01.010 - DOI - PubMed
Aleyasin A, Hosseini MA, Mahdavi A, Safdarian L, Fallahi P, Mohajeri MR et al (2011) Predictive value of the level of vitamin D in follicular fluid on the outcome of assisted reproductive technology. Eur J Obstet Gynecol Reprod Biol 159(1):132–137. https://doi.org/10.1016/j.ejogrb.2011.07.006 - DOI - PubMed
Ozkan S, Jindal S, Greenseid K, Shu J, Zeitlian G, Hickmon C et al (2010) Replete vitamin D stores predict reproductive success following in vitro fertilization. Fertil Steril 94(4):1314–1319. https://doi.org/10.1016/j.fertnstert.2009.05.019 - DOI - PubMed
Anifandis GM, Dafopoulos K, Messini CI, Chalvatzas N, Liakos N, Pournaras S et al (2010) Prognostic value of follicular fluid 25-OH vitamin D and glucose levels in the IVF outcome. Reprod Biol Endocrinol 8:91. https://doi.org/10.1186/1477-7827-8-91 - DOI - PubMed - PMC
Mnallah S, Kacem Berjeb K, Braham M, Khrouf M, Chtourou S, Merdassi G et al (2017) Impact of vitamin D deficiency on ICSI outcomes. JFIV Reprod Med Genet. 5:201. https://doi.org/10.4172/2375-4508.1000201 - DOI
Fabris A, Pacheco A, Cruz M, Puente JM, Fatemi H, Garcia-Velasco JA (2014) Impact of circulating levels of total and bioavailable serum vitamin D on pregnancy rate in egg donation recipients. Fertil Steril 102(6):1608–1612. https://doi.org/10.1016/j.fertnstert.2014.08.030 - DOI - PubMed
Franasiak JM, Molinaro TA, Dubell EK, Scott KL, Ruiz AR, Forman EJ et al (2015) Vitamin D levels do not affect IVF outcomes following the transfer of euploid blastocysts. Am J Obstet Gynecol 212(3):315 e1-315 e6. https://doi.org/10.1016/j.ajog.2014.09.029 - DOI
Neville G, Martyn F, Kilbane M, O’Riordan M, Wingfield M, McKenna M et al (2016) Vitamin D status and fertility outcomes during winter among couples undergoing in vitro fertilization/intracytoplasmic sperm injection. Int J Gynaecol Obstet 135(2):172–176. https://doi.org/10.1016/j.ijgo.2016.04.018 - DOI - PubMed
Abadia L, Gaskins AJ, Chiu YH, Williams PL, Keller M, Wright DL et al (2016) Serum 25-hydroxyvitamin D concentrations and treatment outcomes of women undergoing assisted reproduction. Am J Clin Nutr 104(3):729–735. https://doi.org/10.3945/ajcn.115.126359 - DOI - PubMed - PMC
Merhi Z, Doswell A, Krebs K, Cipolla M (2014) Vitamin D alters genes involved in follicular development and steroidogenesis in human cumulus granulosa cells. J Clin Endocrinol Metab 99(6):E1137–E1145. https://doi.org/10.1210/jc.2013-4161 - DOI - PubMed - PMC
Cunningham TK, Allgar V, Dargham SR, Kilpatrick E, Sathyapalan T, Maguiness S et al (2019) Association of vitamin D metabolites with embryo development and fertilization in women with and without PCOS undergoing subfertility treatment. Front Endocrinol (Lausanne) 10:13. https://doi.org/10.3389/fendo.2019.00013 - DOI
Farzadi L, Khayatzadeh Bidgoli H, Ghojazadeh M, Bahrami Z, Fattahi A, Latifi Z et al (2015) Correlation between follicular fluid 25-OH vitamin D and assisted reproductive outcomes. Iran J Reprod Med 13(6):361–366 - PubMed - PMC
Paffoni A, Ferrari S, Vigano P, Pagliardini L, Papaleo E, Candiani M et al (2014) Vitamin D deficiency and infertility: insights from in vitro fertilization cycles. J Clin Endocrinol Metab 99(11):E2372–E2376. https://doi.org/10.1210/jc.2014-1802 - DOI - PubMed
Garbedian K, Boggild M, Moody J, Liu KE (2013) Effect of vitamin D status on clinical pregnancy rates following in vitro fertilization. CMAJ Open 1(2):E77-82. https://doi.org/10.9778/cmajo.20120032 - DOI - PubMed - PMC
Rudick BJ, Ingles SA, Chung K, Stanczyk FZ, Paulson RJ, Bendikson KA (2014) Influence of vitamin D levels on in vitro fertilization outcomes in donor-recipient cycles. Fertil Steril 101(2):447–452. https://doi.org/10.1016/j.fertnstert.2013.10.008 - DOI - PubMed
Jeppesen JV, Anderson RA, Kelsey TW, Christiansen SL, Kristensen SG, Jayaprakasan K et al (2013) Which follicles make the most anti-Mullerian hormone in humans? Evidence for an abrupt decline in AMH production at the time of follicle selection. Mol Hum Reprod 19(8):519–527. https://doi.org/10.1093/molehr/gat024 - DOI - PubMed
Arefi S, Khalili G, Iranmanesh H, Farifteh F, Hosseini A, Fatemi HM et al (2018) Is the ovarian reserve influenced by vitamin D deficiency and the dress code in an infertile Iranian population? J Ovarian Res 11(1):62. https://doi.org/10.1186/s13048-018-0435-7 - DOI - PubMed - PMC
Gregori S, Casorati M, Amuchastegui S, Smiroldo S, Davalli AM, Adorini L (2001) Regulatory T cells induced by 1 alpha,25-dihydroxyvitamin D3 and mycophenolate mofetil treatment mediate transplantation tolerance. J Immunol 167(4):1945–1953. https://doi.org/10.4049/jimmunol.167.4.1945 - DOI - PubMed
Velthut A, Zilmer M, Zilmer K, Kaart T, Karro H, Salumets A (2013) Elevated blood plasma antioxidant status is favourable for achieving IVF/ICSI pregnancy. Reprod Biomed Online 26(4):345–352. https://doi.org/10.1016/j.rbmo.2012.12.012 - DOI - PubMed
Erel O (2004) A novel automated direct measurement method for total antioxidant capacity using a new generation, more stable ABTS radical cation. Clin Biochem 37(4):277–285. https://doi.org/10.1016/j.clinbiochem.2003.11.015 - DOI - PubMed
Agarwal A, Gupta S, Sharma RK (2005) Role of oxidative stress in female reproduction. Reprod Biol Endocrinol 3:28. https://doi.org/10.1186/1477-7827-3-28 - DOI - PubMed - PMC
Dalto DB, Matte JJ (2017) Pyridoxine (vitamin B(6)) and the glutathione peroxidase system; a link between one-carbon metabolism and antioxidation. Nutrients. https://doi.org/10.3390/nu9030189 - DOI - PubMed - PMC
Nunez-Calonge R, Cortes S, Gutierrez Gonzalez LM, Kireev R, Vara E, Ortega L et al (2016) Oxidative stress in follicular fluid of young women with low response compared with fertile oocyte donors. Reprod Biomed Online 32(4):446–456. https://doi.org/10.1016/j.rbmo.2015.12.010 - DOI - PubMed
Olszak-Wąsik K, Bednarska-Czerwińska A, Olejek A, Tukiendorf A (2019) From, “every day” hormonal to oxidative stress biomarkers in blood and follicular fluid, to embryo quality and pregnancy success? Oxid Med Cell Longev 2019:1092415. https://doi.org/10.1155/2019/1092415 - DOI - PubMed - PMC
Nagy RA, van Montfoort APA, Groen H, Homminga I, Andrei D, Mistry RH et al (2019) Anti-oxidative function of follicular fluid HDL and outcomes of modified natural cycle-IVF. Sci Rep 9(1):12817. https://doi.org/10.1038/s41598-019-49091-3 - DOI - PubMed - PMC
Jain SK, Micinski D (2013) Vitamin D upregulates glutamate cysteine ligase and glutathione reductase, and GSH formation, and decreases ROS and MCP-1 and IL-8 secretion in high-glucose exposed U937 monocytes. Biochem Biophys Res Commun 437(1):7–11. https://doi.org/10.1016/j.bbrc.2013.06.004 - DOI - PubMed - PMC
Tavakoli F, Namakin K, Zardast M (2016) Vitamin D supplementation and high-density lipoprotein cholesterol: a study in healthy school children. Iran J Pediatr 26(4):e3311. https://doi.org/10.5812/ijp.3311 - DOI - PubMed - PMC
Ansari MGA, Sabico S, Clerici M, Khattak MNK, Wani K, Al-Musharaf S et al (2020) Vitamin D supplementation is associated with increased glutathione peroxidase-1 levels in arab adults with prediabetes. Antioxidants (Basel). https://doi.org/10.3390/antiox9020118 - DOI - PubMed - PMC
Francis EC, Hinkle SN, Song Y, Rawal S, Donnelly SR, Zhu Y et al (2018) Longitudinal maternal vitamin D status during pregnancy is associated with neonatal anthropometric measures. Nutrients. https://doi.org/10.3390/nu10111631 - DOI - PubMed - PMC
Leffelaar ER, Vrijkotte TG, van Eijsden M (2010) Maternal early pregnancy vitamin D status in relation to fetal and neonatal growth: results of the multi-ethnic Amsterdam Born Children and their Development cohort. Br J Nutr 104(1):108–117. https://doi.org/10.1017/S000711451000022X - DOI - PubMed
Gernand AD, Simhan HN, Klebanoff MA, Bodnar LM (2013) Maternal serum 25-hydroxyvitamin D and measures of newborn and placental weight in a U.S. multicenter cohort study. J Clin Endocrinol Metab 98(1):398–404. https://doi.org/10.1210/jc.2012-3275 - DOI - PubMed
Aghajafari F, Nagulesapillai T, Ronksley PE, Tough SC, O’Beirne M, Rabi DM (2013) Association between maternal serum 25-hydroxyvitamin D level and pregnancy and neonatal outcomes: systematic review and meta-analysis of observational studies. BMJ 346:f1169. https://doi.org/10.1136/bmj.f1169 - DOI - PubMed
Morley R, Carlin JB, Pasco JA, Wark JD (2006) Maternal 25-hydroxyvitamin D and parathyroid hormone concentrations and offspring birth size. J Clin Endocrinol Metab 91(3):906–912. https://doi.org/10.1210/jc.2005-1479 - DOI - PubMed
Eggemoen ÅR, Jenum AK, Mdala I, Knutsen KV, Lagerløv P, Sletner L (2017) Vitamin D levels during pregnancy and associations with birth weight and body composition of the newborn: a longitudinal multiethnic population-based study. Br J Nutr 117(7):985–993. https://doi.org/10.1017/S000711451700068X - DOI - PubMed
Wei SQ, Qi HP, Luo ZC, Fraser WD (2013) Maternal vitamin D status and adverse pregnancy outcomes: a systematic review and meta-analysis. J Matern Fetal Neonatal Med 26(9):889–899. https://doi.org/10.3109/14767058.2013.765849 - DOI - PubMed
Rudick B, Ingles S, Chung K, Stanczyk F, Paulson R, Bendikson K (2012) Characterizing the influence of vitamin D levels on IVF outcomes. Hum Reprod 27(11):3321–3327. https://doi.org/10.1093/humrep/des280 - DOI - PubMed
Related - In vitro fertilization is more successful when vitamin D in ovaries, not just blood, is increased – April 2022
VitaminDWiki comments
In 2018 the founder of VitaminDWiki asked if it were technically possible to measure vitamin D levels in cells
In 2019 the question was asked again - and the answer then was yes, but it cost about 3X of the serum test
In 2021 most doctors and researchers still only rarely consider the cell levels of vitamin D
5 genes can restrict Vitamin D in the blood from actually getting to the cells
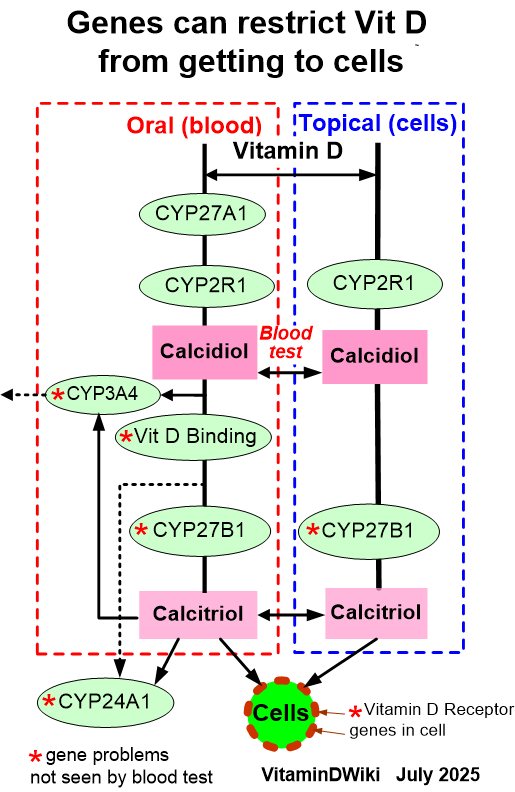
The Vitamin D Receptor is perhaps the most important gene
(the most likely to be deactivated AND the most easily reactivated)
Many diseases have "learned" how to protect themselves by deactivating the Vitamin D Receptor
Many Cancers for example
80-100 ng often gets Vitamin D to the cells even when there are gene restrictions
A normally good level of Vitamin D (e.g. 30 ng) can be restricted by genes however
Vitamin D Receptor category has the following
{include}
VitaminDWiki - Fertility and Sperm category contains
{include}
VitaminDWiki - Vitamin D greatly improves Fertility__
{include}
VitaminDWiki pages with IVF or IN VITRO FERTILIZATION in title (13 as of April 2022)
This list is automatcially updated
{LIST()}
{list max="50"}
{sort mode="modificationdatemajor_desc"}
{OUTPUT(template="table")}
{tableparams allowtableexpansion="n" shownbitems="y" title=""}
{column sort="title" label="Title" field="title" mode="raw"}{column}
{column label="Modified" sort="modificationdatemajor" field="modificationdatemajor"}
{OUTPUT}
{FORMAT(name="title")}{display name=title format="objectlink"}{FORMAT}
{FORMAT(na
Title change made April 2022 caused the visitor count to reset.
There have actually been visitors to this page since it was originally made
