Advanced Colorectal Cancer survival is increased somewhat with 4,000 IU of vitamin D – RCT
Effect of High-Dose vs Standard-Dose Vitamin D3 Supplementation on Progression-Free Survival
Among Patients With Advanced or Metastatic Colorectal Cancer -The SUNSHINE Randomized Clinical Trial
JAMA. 2019;321(14):1370-1379. doi:10.1001/jama.2019.2402
 * Chemotheraphy not work as well with low Vitamin D (colon cancer this time) – Aug 2018
* Note: 4,000 IU daily dosing would NOT have helped Chemotherapy - would have taken months to increase the vitamin D levels
---
1. Vitamin D Receptor and Cancers
1. Items in both categories Vitamin D Receptor and Cancer - Colon:
{category}
1. Items in both categories Vitamin D Receptor and Cancer
{category}
* Chemotheraphy not work as well with low Vitamin D (colon cancer this time) – Aug 2018
* Note: 4,000 IU daily dosing would NOT have helped Chemotherapy - would have taken months to increase the vitamin D levels
---
1. Vitamin D Receptor and Cancers
1. Items in both categories Vitamin D Receptor and Cancer - Colon:
{category}
1. Items in both categories Vitamin D Receptor and Cancer
{category}
📄 Download the PDF from VitaminDWiki
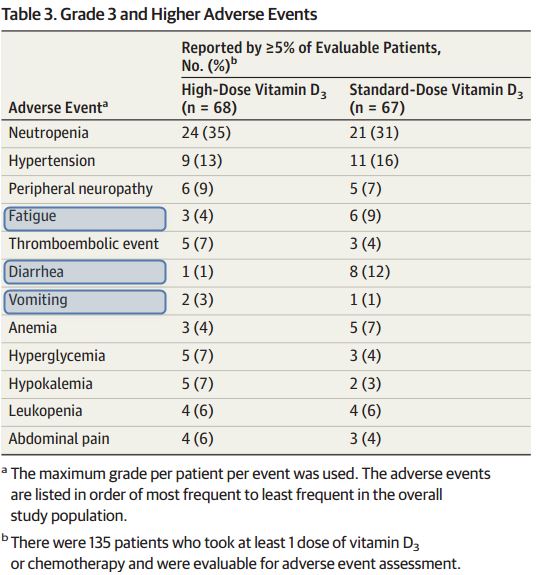
Fewer adverse effects if get Vitamin D
Key Points
Question Does high-dose vitamin D3 supplementation prolong progression-free survival when added to standard chemotherapy in patients with advanced or metastatic colorectal cancer?
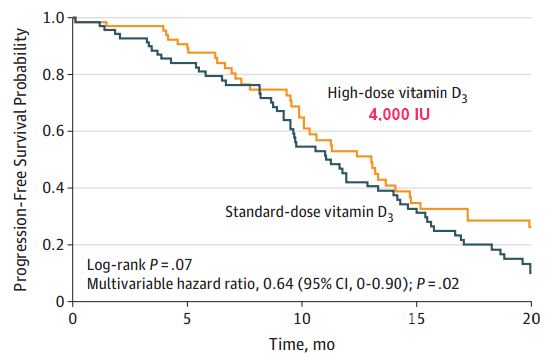
Findings In this phase 2 randomized clinical trial that included 139 patients with advanced or metastatic colorectal cancer, treatment with chemotherapy plus high-dose vitamin D3 supplementation vs chemotherapy plus standard-dose vitamin D3 resulted in a median progression-free survival of 13 months vs 11 months , respectively, that was not statistically significant, but a multivariable hazard ratio of 0.64 for progression-free survival or death that was statistically significant.
Meaning These findings regarding a potential role for high-dose vitamin D3 supplementation in the treatment of patients with advanced or metastatic colorectal cancer warrant further evaluation in a larger multicenter randomized clinical trial.
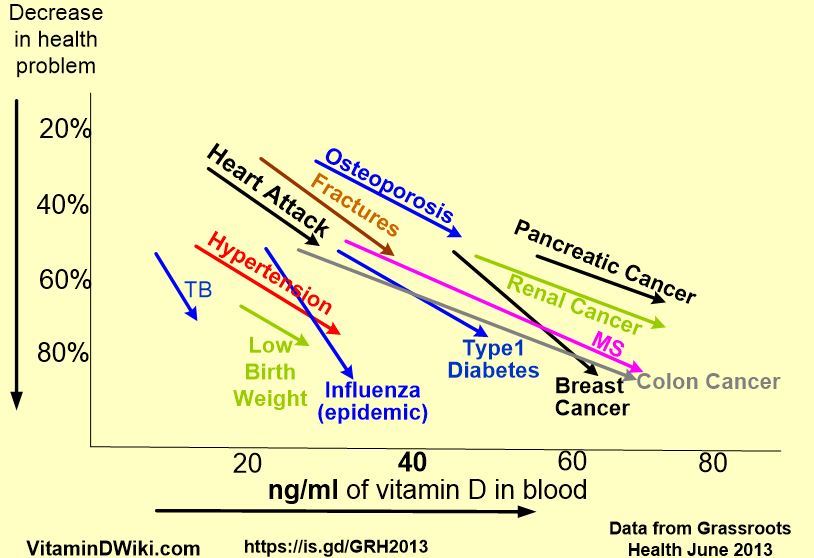
Importance In observational studies, higher plasma 25-hydroxyvitamin D (25[OH]D) levels have been associated with improved survival in metastatic colorectal cancer (CRC).
Objective To determine if high-dose vitamin D3 added to standard chemotherapy improves outcomes in patients with metastatic CRC.
Design, Setting, and Participants Double-blind phase 2 randomized clinical trial of 139 patients with advanced or metastatic CRC conducted at 11 US academic and community cancer centers from March 2012 through November 2016 (database lock: September 2018).
Interventions mFOLFOX6 plus bevacizumab chemotherapy every 2 weeks and either high-dose vitamin D3 (n = 69) or standard-dose vitamin D3 (n = 70) daily until disease progression, intolerable toxicity, or withdrawal of consent.
Main Outcomes and Measures The primary end point was progression-free survival (PFS) assessed by the log-rank test and a supportive Cox proportional hazards model. Testing was 1-sided. Secondary end points included tumor objective response rate (ORR), overall survival (OS), and change in plasma 25(OH)D level.
Results Among 139 patients (mean age, 56 years; 60 [43%] women) who completed or discontinued chemotherapy and vitamin D3 (median follow-up, 22.9 months), the median PFS for high-dose vitamin D3 was 13.0 months (95% CI, 10.1 to 14.7; 49 PFS events) vs 11.0 months (95% CI, 9.5 to 14.0; 62 PFS events) for standard-dose vitamin D3 (log-rank P = .07); multivariable hazard ratio for PFS or death was 0.64 (1-sided 95% CI, 0 to 0.90; P = .02). There were no significant differences between high-dose and standard-dose vitamin D3 for tumor ORR (58% vs 63%, respectively; difference, −5% [95% CI, −20% to 100%], P = .27) or OS (median, 24.3 months vs 24.3 months; log-rank P = .43). The median 25(OH)D level at baseline for high-dose vitamin D3 was 16.1 ng/mL vs 18.7 ng/mL for standard-dose vitamin D3 (difference, −2.6 ng/mL [95% CI, −6.6 to 1.4], P = .30); at first restaging, 32.0 ng/mL vs 18.7 ng/mL (difference, 12.8 ng/mL [95% CI, 9.0 to 16.6], P < .001); at second restaging, 35.2 ng/mL vs 18.5 ng/mL (difference, 16.7 ng/mL [95% CI, 10.9 to 22.5], P < .001); and at treatment discontinuation, 34.8 ng/mL vs 18.7 ng/mL (difference, 16.2 ng/mL [95% CI, 9.9 to 22.4], P < .001). The most common grade 3 and higher adverse events for chemotherapy plus high-dose vs standard-dose vitamin D3 were neutropenia (n = 24 [35%] vs n = 21 [31%], respectively) and hypertension (n = 9 [13%] vs n = 11 [16%]).
Conclusions and Relevance Among patients with metastatic CRC, addition of high-dose vitamin D3, vs standard-dose vitamin D3, to standard chemotherapy resulted in a difference in median PFS that was not statistically significant, but with a significantly improved supportive hazard ratio. These findings warrant further evaluation in a larger multicenter randomized clinical trial.
