Australians paying for most Vitamin D tests, 40 percent deficient in winter
Changes to the frequency and appropriateness of vitamin D testing after the introduction of new Medicare criteria for rebates in Australian general practice: evidence from 1.5 million patients in the NPS Medicine Insight database
BMJ Open http://dx.doi.org/10.1136/bmjopen-2018-024797
David Gonzalez-Chica1,2, Nigel Stocks1
📄 Download the PDF from VitaminDWiki
40% of Australians who had to pay for their own Vitamin D test
(no medical reason/justification) were found to have<20 ng of vitamin D in the winter
Lots of Vitamin D deficiency far from the equator

Note: Melborne latitude = 38 degrees = San Francisco
Objectives To assess changes in the frequency of vitamin D testing and detection of moderate/severe vitamin D deficiency (<30 nmol/L) among adults after the introduction of new Medicare Benefits Schedule (MBS) rebate criteria (November 2014), and their relationship to sociodemographic and clinical characteristics.
Design Dynamic (open) cohort study
Setting Primary care
Participants About 1.5 million ‘active’ patients aged 18+ years visiting a general practitioner and included in the National Prescribing Service Medicine Insight database.
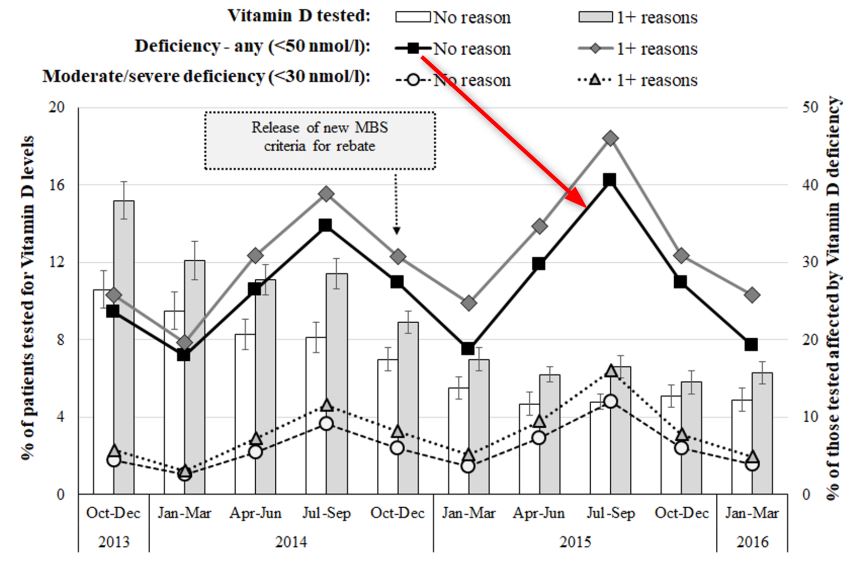
Outcome measures The frequency of vitamin D testing (per 1000 consultations) and moderate/severe vitamin D deficiency (%) recorded between October 2013 and March 2016, stratified by the release of the new MBS criteria for rebate.
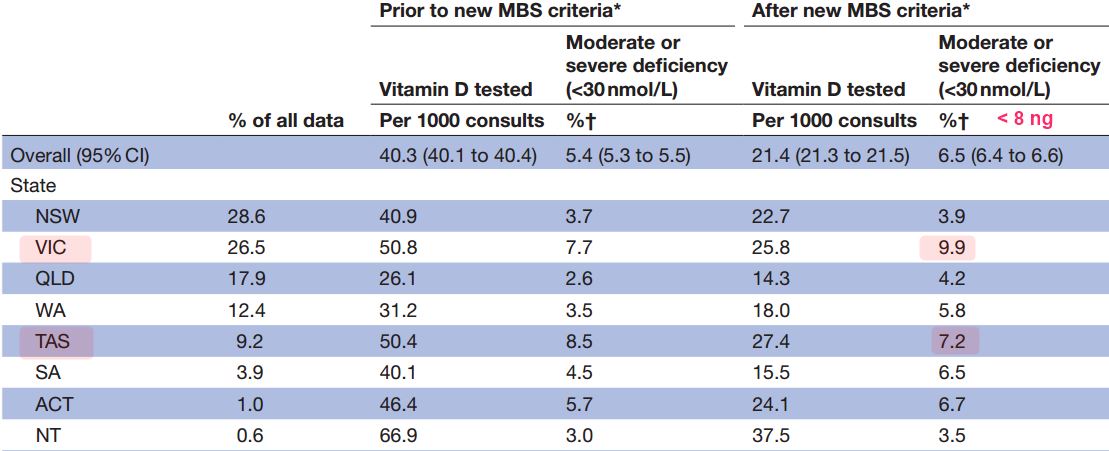
Results More patients were female (57.7%) and 30.2% were aged 60+ years. Vitamin D testing decreased 47% (from 40.3 to 21.4 tests per 1000 consultations) after the new MBS criteria, while the proportion of tests with no indication for being performed increased from 71.3% to 76.5%. The proportion of patients identified as moderate/severe vitamin D deficient among those tested increased from 5.4% to 6.5%. Practices located in high socioeconomic areas continued to have the highest rates of testing, but moderate/severe vitamin D deficiency detection remained 90% more frequent in practices from low socioeconomic areas after the rebate change. Furthermore, the frequency of individuals being tested was reduced independent of the patients’ sociodemographic or clinical condition, and the gap in the prevalence of vitamin D deficiency detection between those meeting or not meeting the criteria for being tested remained the same. Moderate/severe vitamin D deficiency detection decreased slightly among patients with hyperparathyroidism or chronic renal failure.
Conclusions Although the new criteria for rebate almost halved the frequency of vitamin D testing, it also lessened the frequency of testing among those at higher risk of deficiency, with only a small improvement in vitamin D deficiency detection.
Conclusions (from PDF)
Although the new criteria for rebate almost halved the frequency of vitamin D testing, it also
lessened the frequency of testing among those at highest risk of deficiency,
increased the proportion of tests with no indication for being performed, and
resulted in only a small improvement in the detection of vitamin D deficiency.
Therefore, despite a marked reduction in healthcare(testing) costs,
the introduction of the new MBS criteria for rebate resulted in some unintended consequences : the changes
did not improve the appropriateness of vitamin D testing,
did not provide additional benefits for those at a higher risk of vitamin D deficiency and
did not reduce health disparities in Australian general practice.
Further studies could explore the ongoing, non-financial, health costs of these changes and develop practice, GP and patient-centric interventions to improve the appropriateness of vitamin D testing.
