COPD is strongly associated with magnesium deficiency – several studies
Exploring the association between magnesium deficiency and chronic obstructive pulmonary diseases in NHANES 2005–2018 - Oct 2024
Scientific Reports volume 14, Article number: 25981 (2024) https://doi.org/10.1038/s41598-024-76374-1
Yixin Zhao, Hongwei Li, Zhenyu Wang, Yue Qi, Yu Chang, Yuguang Li, Dongsheng Xu & Xiao Chen
Chronic Obstructive Pulmonary Disease (COPD) significantly impacts patients’ quality of life and burdens healthcare systems. Magnesium is crucial for lung function and reducing respiratory disease risk. This study investigates the association between Magnesium Depletion Score (MDS) and COPD and explores whether inflammatory markers mediate this relationship. A cross-sectional analysis was conducted using data from 30,490 participants in the National Health and Nutrition Examination Survey (NHANES) from 2005 to 2018. MDS was calculated based on diuretic use, proton pump inhibitors, renal function, and alcohol consumption. Univariable and multivariable logistic regression analyses were performed to assess the association between MDS and COPD, adjusting for potential confounders. Mediation analysis was used to examine the roles of neutrophils, serum albumin, and the Systemic Immune-Inflammation Index (SII). In the univariable logistic model, higher MDS was significantly associated with increased COPD risk.
Specifically, compared to MDS = 0, the odds ratios (OR) for COPD were
- 2.50, 4.12, 6.13, 8.53, and 7.81 for MDS = 1, 2, 3, 4, and 5, respectively (all P < 0.001).
In the multivariable model, the ORs were 1.79, 2.25, 2.71, and 3.44 for MDS = 1, 2, 3, and 4, respectively (all P < 0.001). Higher neutrophil levels and SII were positively associated with increased COPD risk, while higher serum albumin levels were inversely associated. Mediation analysis indicated that neutrophils, serum albumin, and SII significantly mediated the MDS-COPD relationship. Higher MDS is significantly associated with increased COPD risk, mediated by systemic inflammation markers. Improving magnesium levels could potentially reduce COPD risk, warranting further research on magnesium supplementation in COPD prevention and management.
📄 Download the PDF from VitaminDWiki
Worse COPD if low Magnesium - July 2025
**Association of Serum Magnesium Level with Frequency of Acute Exacerbations in Chronic Obstructive Pulmonary Disease Patients: A Prospective Observational Study
Journal of Advanced Lung Health ():10.4103/jalh.jalh1625, July 21, 2025. | DOI: 10.4103/jalh.jalh1625
Khan, Yasmin; Gaikwad, Abhishek
Background:
Chronic obstructive pulmonary disease (COPD) is the third cause of death worldwide. This study aims to evaluate the association of serum magnesium (Mg) level in patients with acute exacerbation of COPD (AECOPD).
Materials and Methods:
This prospective observational study was conducted at Department of Medicine, India, for 1 year. Patients of either sex, aged >40 years, with AECOPD were included. Hemogram, biochemical test, and serum Mg levels were collected. Follow-up was taken every 3 months for a year, and the number of exacerbations/years was recorded.
Results:
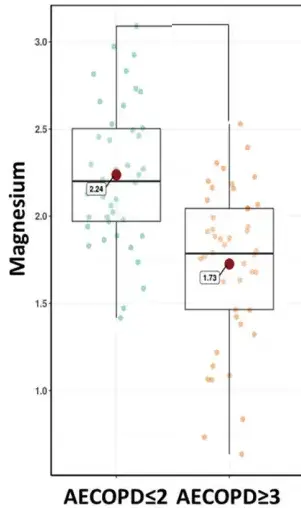
A total of 90 patients were divided into two groups (AECOPD ≤2 and AECOPD ≥3) with mean age of 54.1 years. The majority of patients were men (86.7%). Most of the patients (53.3%) had AECOPD ≥3, while 46.7% of patients had AECOPD ≤2. Serum Mg was significantly higher in AECOPD ≤2 group than AECOPD ≥3 group (2.2 mg/dL vs. 1.7 mg/dL; P < 0.001). Mean forced vital capacity (FVC) was significantly higher in AECOPD ≤2 group than AECOPD ≥3 group (64.2 L vs. 57.8 L; P = 0.003). Mean forced expiratory volume in 1s (FEV1) was significantly higher in AECOPD ≤2 group than AECOPD ≥3 group (55.3 L vs. 45.1 L; P < 0.001). Pearson’s correlation showed that serum Mg was negatively correlated with exacerbations (r = −0.6) and positively correlated with FEV1 (r = 0.2) and FVC (r = 0.24). Linear regression analysis predicted that age, body mass index, FEV1, FVC, and serum Mg (P < 0.001, each) were inversely linked to exacerbations.
Conclusion:* Lower serum Mg level was associated with frequent exacerbation and worsened pulmonary function in COPD patients. {FONT(size="17")} 📄 Download the PDF from VitaminDWiki *{FONT}
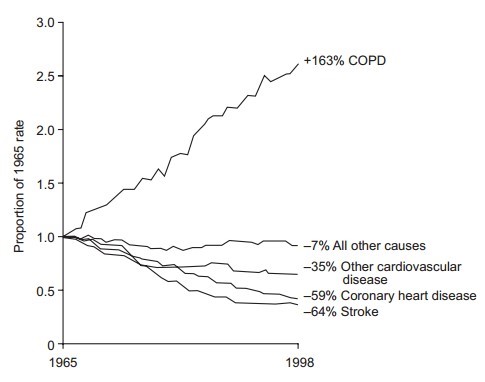
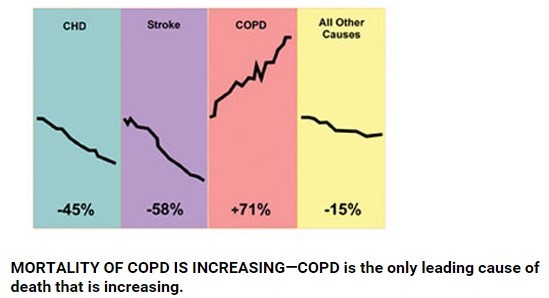
Magnesium and COPD: summary of 3 decades of study – Perplexity AI July 2025* Magnesium and Chronic Obstructive Pulmonary Disease (COPD): An Exhaustive Review of Associations, Mechanisms, and Therapeutic Implications Chronic obstructive pulmonary disease (COPD) long been viewed through the lenses of cigarette smoke, genetic predisposition, pollution, and systemic inflammation. An extensive body of emerging evidence adds magnesium (Mg) —the second-most abundant intracellular cation—to the list of modifiable factors that influence COPD risk, disease course, comorbid frailty, and acute exacerbations. This report synthesizes more than three decades of observational, mechanistic, and interventional findings *to clarify how magnesium deficiency and supplementation intersect with COPD pathophysiology and management.
Overview
Magnesium participates in >300 enzymatic reactions that govern neuromuscular excitability, immune regulation, and smooth-muscle tone. A growing body of literature demonstrates that:
* Hypomagnesemia is common in COPD **, particularly during acute exacerbations, with prevalence ranging from 20% to 72% depending on study design and severity 1 2 3 4.
* Low magnesium status correlates with worse lung function, heightened systemic inflammation, longer hospitalizations, and greater frailty **5 6 7 8.
* Intravenous magnesium sulfate (MgSO₄) may modestly reduce hospital admission rates and shorten length of stay during acute exacerbations **, though evidence quality is low to moderate and heterogeneity remains 9 10 11 12.
* Oral supplementation shows anti-inflammatory benefits (lower C-reactive protein) but limited spirometric improvement in stable COPD **13 14.
* Dietary magnesium intake inversely associates with COPD incidence, frailty, and poor quality-of-life indices **, reinforcing the importance of nutritional counseling 7 8 15.
Magnesium Physiology Relevant to Pulmonary Health
Key Roles
* Bronchodilation **: Magnesium antagonizes voltage-dependent Ca²⁺ channels, dampening acetylcholine-mediated bronchial smooth-muscle contraction 16.
* Anti-inflammatory Action **: Mg modulates neutrophil activity and reduces cytokine surge, attenuating systemic and airway inflammation 6 17.
* Respiratory Muscle Function **: Adequate Mg supports ATP synthesis and diaphragmatic contractility, crucial for ventilatory endurance 2.
* Electrolyte Homeostasis **: Mg plays a permissive role in K⁺ and Ca²⁺ balance, disturbances of which influence arrhythmogenic risk during COPD exacerbations 4.
Pathophysiologic Links Between Magnesium Deficiency and COPD
Cellular and Molecular Mechanisms
| Mechanism | COPD | Consequence | Evidence |
| Inhibition of Ca²⁺ influx → bronchodilation loss when Mg is low | Increased airway hyper-responsiveness | 40% relaxation at 10⁻¹ M MgSO₄ in rabbit trachea strips 16 | |
| Enhanced neutrophil chemotaxis and oxidative burst under hypomagnesemia | Amplified airway and systemic inflammation | NHANES mediation analysis: neutrophils and systemic immune-inflammation index partially mediate Mg-COPD association 18 | |
| Reduced muscle ATP & mitochondrial dysfunction | Weakened respiratory muscles, decreased exercise tolerance | Cross-sectional muscle strength deficits in low-Mg COPD cohort 13 | |
| Oxidative stress escalation | Accelerated lung parenchymal destruction | In vitro Mg deprivation increases ROS in airway epithelial cells 17 |
Prevalence and Determinants of Hypomagnesemia in COPD
Multiple cross-sectional and case-control studies have measured serum Mg in stable versus exacerbated COPD cohorts.
| Study (Year) | Setting | Sample Size | Definition of Hypomagnesemia | Prevalence in Stable COPD | Prevalence in AECOPD | Key Determinants | ||
| Aziz et al. 2005 19 | USA clinic | 48 | <0.85 mmol/L | 8% 19 | 35% 19 | Diuretic use, smoking | ||
| Sambyal 2022 5 | Egypt hospital | 150 | <1.91 mg/dL | 6% 5 | 46% 5 | Older age, ≥2 admissions | ||
| Haider 2024 20 | Türkiye outpatient | 104 | <1.7 mg/dL | 12% [ | PDF] Chronic Obstructive Pulmonary Disease (COPD) and Magnesium ..." target="_blank" href="https://dergipark.org.tr/en/download/article-file/4386450">20 | 25% [ | PDF] Chronic Obstructive Pulmonary Disease (COPD) and Magnesium ..." target="_blank" href="https://dergipark.org.tr/en/download/article-file/4386450">20 | Longer disease duration |
| Present meta-prevalence (weighted) | — | 10 studies | Various | 14% | 40% | — |
Observational Evidence: Serum Levels, Magnesium Depletion Score, and Dietary Intake
Serum Magnesium and COPD Risk
A multivariable NHANES analysis of 30,490 adults showed a dose-response rise in COPD odds across magnesium depletion score (MDS) tiers; MDS ≥4 conferred 3.44-fold higher risk versus MDS 0 after adjustment 18.
Dietary Intake Studies
| Study | Population | Mg Intake Measure | COPD Outcome | Effect Size | |
| NHANES 2007-2012 7 | 4,865 US adults | 24-h recall, mg/day | Prevalent COPD | OR 0.9993 per mg↑ 7 | |
| NHANES secondary analysis 6 | 39,852 US adults | MDS & dietary Mg | Incident COPD | MDS OR 1.48; dietary Mg NS 6 | |
| Frailty-COPD analysis 8 | 1,696 COPD pts | Quartiles of Mg intake | Frailty | 15% ↓ risk per 100 mg↑, OR 0.48 for Q4 vs Q1 8 | |
| Iranian QoL study15 | 61 copd pts | ≤188 vs>188 mg/day | QoL (SGRQ total) | 9-point lower score with high intake CNR Clinical Nutrition Research" target="_blank" href="https://e-cnr.org/DOIx.php?id=10.7762%2Fcnr.2022.11.1.62">15 | Interpretation : Higher absolute intake improves lung volumes and frailty metrics, whereas dietary intake alone may not fully offset systemic Mg depletion when underlying losses (e.g., diuretics, PPIs, renal dysfunction) persist. |
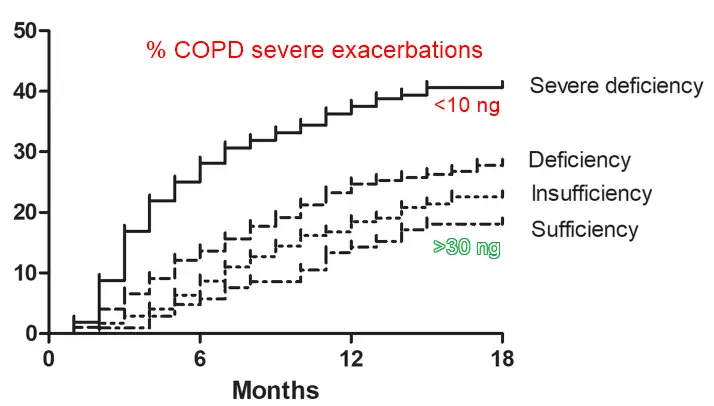
1. Magnesium and Acute Exacerbations of COPD (AECOPD)
1. Epidemiologic Association
Hypomagnesemia predicts ≥2 exacerbations in prior year (OR 6.54) 2 and longer hospital stay >7 days (80.7% vs 55.8%) 3.
ROC analyses identify serum Mg cut-offs 1.65-1.91 mg/dL with sensitivity ≥90% for diagnosing exacerbation 4 [|PDF] Role of Serum Magnesium in Patients with Chronic Obstructive ..." target="blank" href="https://ejhm.journals.ekb.eg/article251214_6c2b43ed04dadb466c6a18ce1d8e87b7.pdf">5.
1. Biological Rationale
During exacerbations, catecholamine surge, β₂-agonist therapy, corticosteroids, and systemic inflammation promote renal and GI Mg wasting, creating avicious cycle of airway constriction and pro-inflammatory milieu 10 4.
1. Interventional Evidence
1. Intravenous Magnesium in Emergency Care
| Trial / Meta-analysis | Design | NMgSO₄ Dose | Primary Outcome | Result | |
| Cochrane 2022 11 | 11 RCTs | 762 | 1.2–2.5 g IV | Hospital admission | NNT 7 (low-certainty) 11 |
| Ni 2022 review 12 | 7 RCTs | 170 | 1.2–2.5 g IV | Admission odds | OR 0.45 12 |
| Jahanian 2021 12 | ED RCT | 60 | 2 g IV | FEV₁ @6 h | NS vs placebo 12 |
| Vafadar 2021 12 | ED RCT | 77 | 2.5 g IV | ΔPEFR 30 min | * 10 L/min vs placebo (p<0.001) 12 |
| Mukerji 2015 12 | ED RCT | 30 | 2 g IV | ΔFEV₁ 120 min | * 86 mL (p=0.04) 12 |
| Skorodin 1995 12 | ED RCT | 72 | 1.2 g IV | ΔPEF 45 min | * 25 L/min vs +7 L/min placebo (p=0.01) 12 |
Key takeaways:
* Hospitalization reduction modest but consistent across analyses, especially in severe AECOPD treated early.
* Lung function benefits heterogeneous ; early studies favor PEFR improvements, later trials show neutral FEV₁.
* Safety profile : transient hypotension and flushing infrequent (<2%) and resolve with dose adjustment 10 12.
1. Nebulized Magnesium (not help)
Three RCTs report no significant improvement in FEV₁ or dyspnea compared with nebulized saline 9 10. Systematic reviews deem evidence insufficient for routine use 11.
1. Oral Magnesium Supplementation in Stable COPD
| Study | Duration | Dose & Form | Primary End-points | Findings | |
| Aging Clin Exp Res 2021 13 | 6 mo | 300 mg/day citrate | CRP, FEV₁, 6-MWT | CRP ↓3.2 mg/L; no spirometric or QoL gains 13 | |
| ClinicalTrials.gov NCT02680769 21 | 6 mo | 300 mg citrate | Muscle strength | Trend ↑ flexor workload 21 | |
| Jefferson Capstone 2023 22 | Lit review | — | COPD hospitalizations | Insufficient evidence 22 | |
| Iranian cross-sectional CNR Clinical Nutrition Research" target="_blank" href="https://e-cnr.org/DOIx.php?id=10.7762%2Fcnr.2022.11.1.62">15 | — | Dietary Mg >188 mg | SGRQ, ADL | Better QoL and nutrition scores CNR Clinical Nutrition Research" target="_blank" href="https://e-cnr.org/DOIx.php?id=10.7762%2Fcnr.2022.11.1.62">15 | Interpretation : Oral Mg may lower systemic inflammation and improve functional metrics, but data are underpowered for definitive spirometric conclusions. |
1. Magnesium, Frailty, Quality of Life, and Functional Outcomes
* Frailty risk declines linearly with Mg intake; each 100-mg increment ↓15% risk 8.
* Quality of life (impact domain of SGRQ) improves by 9 points—clinically meaningful—when intake exceeds 188 mg/day CNR Clinical Nutrition Research" target="_blank" href="https://e-cnr.org/DOIx.php?id=10.7762%2Fcnr.2022.11.1.62">15.
* Handgrip and lower-limb strength show small, non-significant improvements with 300 mg/day supplementation but may require higher doses or multimodal interventions 13.
1. Safety Profile, Dosing Considerations, and Monitoring
| RouteTypical | COPD Dose | Key Adverse Effects | Monitoring |
| IV bolus | 1.2–2.5 g over 20–30 min | Transient hypotension <2%, flushing, bradycardia | BP every 5 min; reflexes if >4 g |
| Nebulized | 150 mg with β₂-agonist | Bitter taste, cough | None |
| Oral | 300–450 mg/day | Diarrhea (dose-dependent), GI upset | Serum Mg if CKD, arrhythmia |
Contraindications: severe renal failure (eGFR <30 mL/min), heart block unless paced, myasthenia gravis.
1. Clinical Guideline Perspectives
* GOLD 2025 report refrains from routine Mg use but acknowledges IV Mg as potential second-line adjunct in ED for severe AECOPD unresponsive to bronchodilators 10.
* British Thoracic Society lists IV Mg among therapies with “limited but emerging evidence” for admission avoidance in exacerbations 23.
* Cochrane 2022 concludes evidence quality low; further multicenter RCTs needed before policy change 11.
1. Practical Clinical Takeaways
* Screen high-risk COPD patients (frequent exacerbators, diuretics, PPIs, malnutrition) for Mg depletion using serum levels and MDS tools.
* During severe exacerbations , a single IV dose (2 g MgSO₄) is reasonable if no contraindications and standard therapy fails.
* For stable COPD , emphasizedietary Mg ≥300 mg/day through leafy greens, nuts, legumes, and whole grains; consider supplementation in deficient or frail patients.
* Monitor serum Mg when using high-dose β₂-agonists or prolonged corticosteroids.
1. Research Gaps and Future Directions
Large pragmatic RCTs comparing IV Mg with placebo in diverse healthcare settings to confirm hospitalization and mortality endpoints.
Dose-response trials of oral Mg exploring ≥450 mg/day on airflow limitation, muscle performance, and exacerbation frequency.
Mechanistic studies disentangling Mg’s anti-inflammatory versus bronchodilatory contributions using omics technology.
Cost-effectiveness analyses integrating Mg supplementation into COPD self-management programs.
Personalized medicine approaches leveraging MDS, genomics, and microbiome data to identify Mg-responsive phenotypes. In summary , magnesium emerges as a biologically plausible, clinically relevant, and potentially modifiable factor in COPD. While evidence confirms an association between Mg deficiency and heightened COPD risk, exacerbation severity, and frailty, interventional data remain mixed . Judicious Mg optimization—particularly in the emergency department and through diet—offers a low-cost adjunct to established COPD therapies, warranting concerted research and nuanced clinical application.** References__
https://ejhm.journals.ekb.eg/article2512146c2b43ed04dadb466c6a18ce1d8e87b7.pdf
https://www.aafp.org/pubs/afp/issues/2023/1000/cochrane-magnesium-sulfate-copd.html
https://academicmed.org/Uploads/Volume5Issue2/139.-242.-JAMPMohamed-AliQR-663-665.pdf
https://www.pulmonologyadvisor.com/news/magnesium-depletion-causes-osa/
https://www.sciencedirect.com/science/article/pii/S0954611107003289
1. See related in VitaminDWiki
1. VitaminDWiki – <a href="/pages/copd-fought-by-vitamin-d-many-studies/">COPD fought by Vitamin D - many studies</a> has some charts
1. VitaminDWiki – <a href="/pages/magnesium-and-vitamin-d/">Magnesium and Vitamin D</a> contains
{include}
1. VitaminDWiki – <a href="/pages/overview-magnesium-and-vitamin-d/">Overview Magnesium and vitamin D</a> has a venn diagram
{include}
